Paxlovid and Long Covid
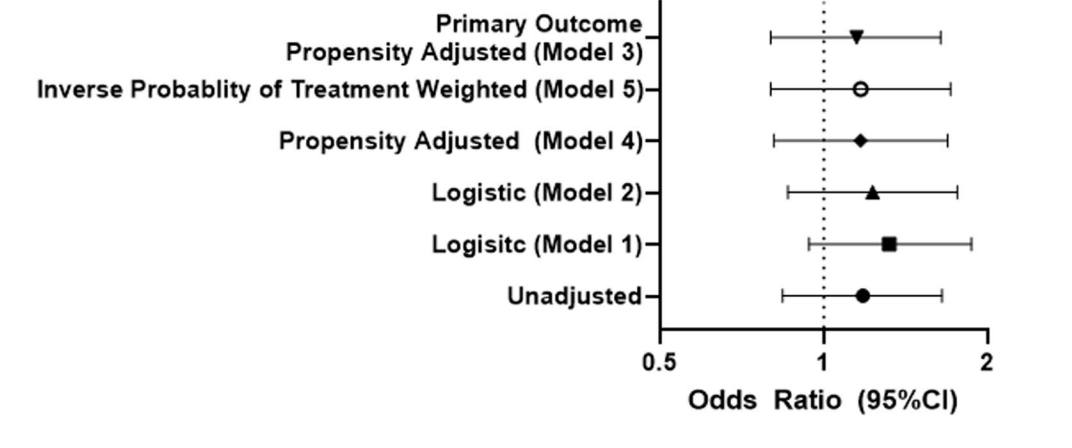
Paxlovid might help shorten and diminish a COVID infection, but the antiviral doesn’t reduce the risk of developing long COVID.
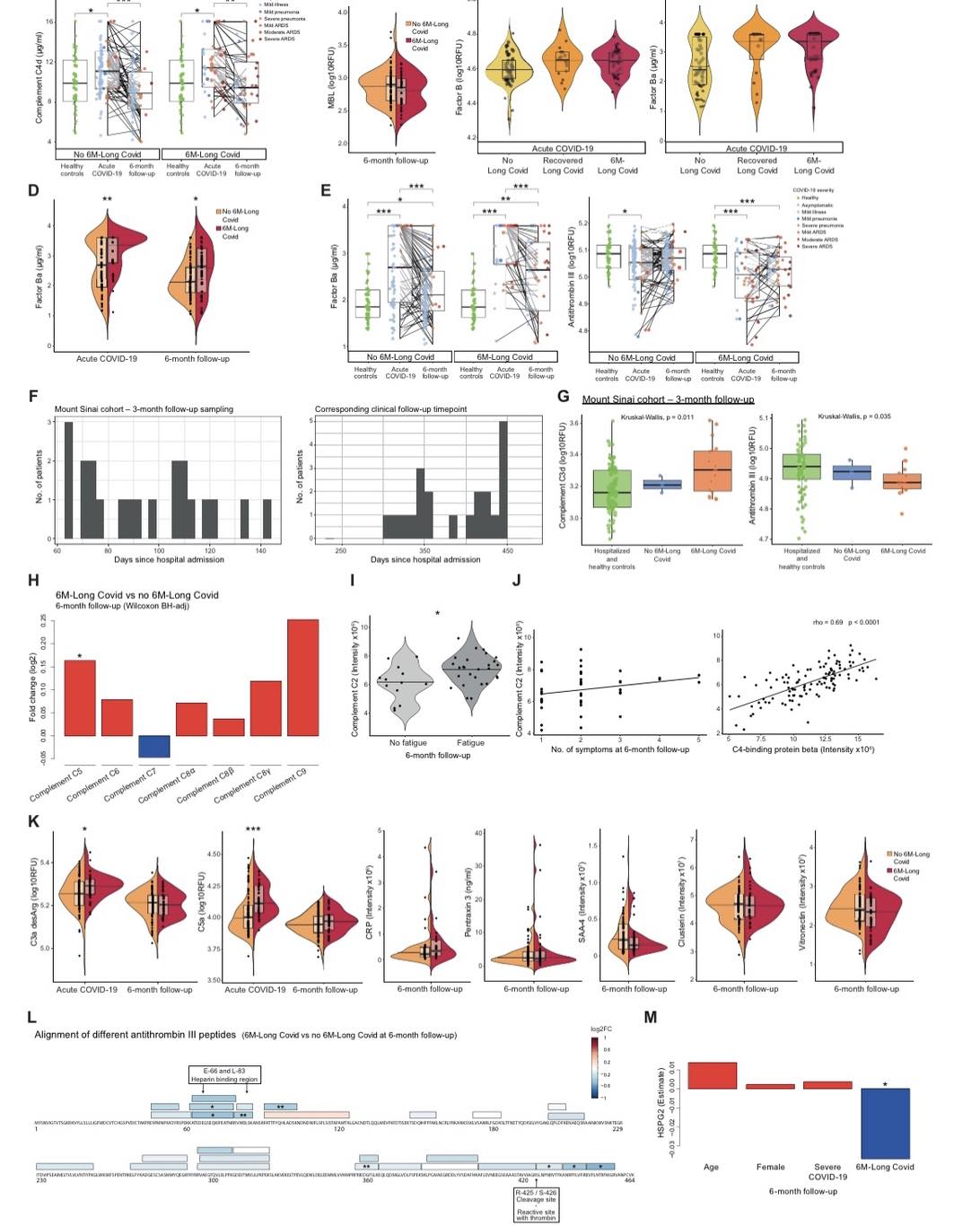
The Study“Top candidate biomarkers were identified”
“Scientists have identified a persistent change in a handful of blood proteins in people with long Covid that indicates that an important part of their immune system remains on high alert for months after an acute infection.
These findings, published Thursday in the journal Science, could help explain what causes the persistent fatigue, brain fog and other debilitating symptoms of long Covid, as well as pave the way for diagnostic tests and potentially, a long-awaited treatment”

Being vaccinated reduces the chance of long covid.
“Vaccination against COVID-19 consistently reduced the risk of long COVID symptoms, which highlights the importance of vaccination to prevent persistent COVID-19 symptoms, particularly in adults”
The study included over 10million vaccinated people, and another 10million unvaccinated people. So these results are very reliable.
The evidence to support HBOT is weak, any benefit is likely short term and very expensive. Probably best avoided unless better evidence comes along.
More information463 participants, Double blinded, placebo controlled trail.
Very promising results for the use of synbiotic supplements against long covid. This is the most promising data I have seen so far for anything against long covid.
Very encouraging results for alleviation of:
fatigue (p=0·0001, 0.01%),
memory loss (p=0·0024, 0.24%),
difficulty in concentration (p<0·0001, less than 0.01%),
gastrointestinal upset (p=0·0014, 0.14%),
and general unwellness (p=0·0008, 0.08%)
compared with the placebo group.
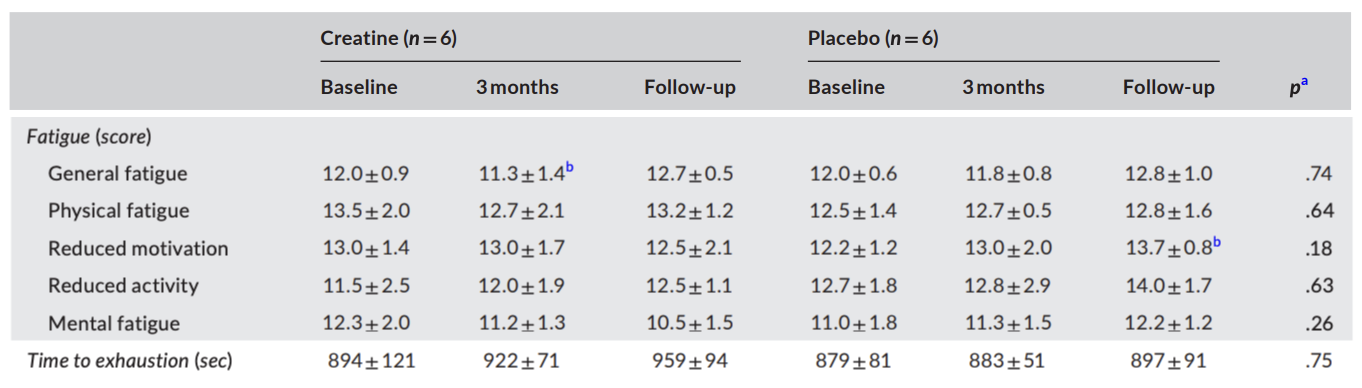
Creatine supplements
Taking a daily creatine supplement, 4g of creatine monohydrate per day.
Only 12 people in the study, this is a major limitation. 6 taking creatine and 6 placebo, with the age of participants of the placebo group being significantly lower 23.3 ± 2.0 than the treatment group. 31.7 ± 9.4. But matched well in other areas.
With multiple measurements of subjective levels of fatigue, it is like they are fishing for significance, more on this later. However, I do like that they included an objective measure with time to exhaustion.
Objective measure are always going to be more reliable that subjective ones, as they are less susceptible to bias. However, this is only how they can withstand short term excursion. The best method would be to attach smart watch/fitbits to all participants and measure the activity levels over the courser of the study.
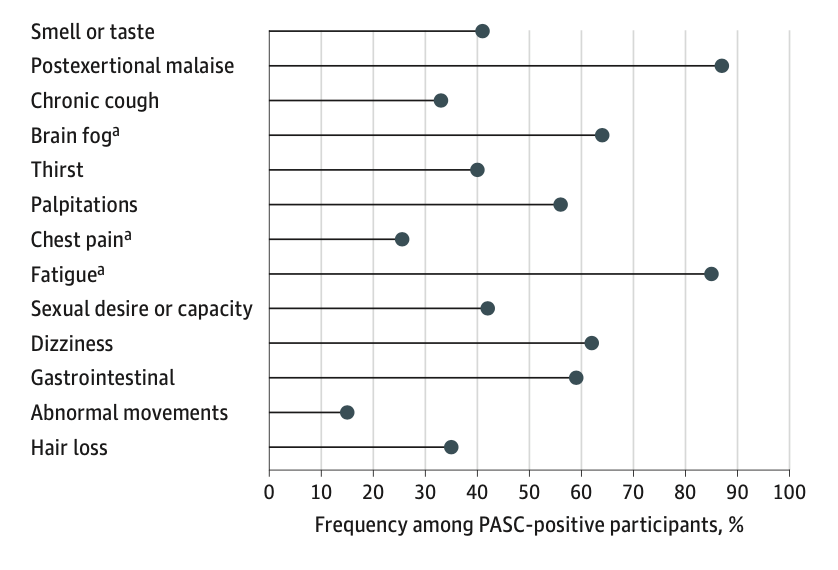
Twelve main Symptoms of Long Covid
Prospective study with a total of 9764 participants, 8637 comfirmed infection with covid-19, was used to create a definition of LC based on Symptoms.
postexertional malaise, fatigue, brain fog, dizziness, gastrointestinal symptoms, palpitations, changes in sexual desire or capacity, loss of or change in smell or taste, thirst, chronic cough, chest pain, and abnormal movements.
(Infected% vs uninfected%, adjusted odds ratio, [Confidence interval])
Postexertional malaise (PEM) (28% vs 7%; aOR, 5.2 [95% CI, 3.9-6.8]),
fatigue (38% vs 17%; aOR, 2.9 [95% CI, 2.4-3.4]),
dizziness (23% vs 7%; aOR, 3.4 [95% CI, 2.6-4.4]),
brain fog (20% vs 4%; aOR, 4.5 [95% CI, 3.2-6.2]), and
gastrointestinal (GI) symptoms (25% vs 10%; aOR, 2.7 [95% CI, 2.2-3.4])
Hyperbaric oxygen therapy (HBOT)
Unpeer reviewed, unpublished data presented at a conference showed a weak positive result for HBOT.
"In the HBOT group, GLS increased significantly from –17.8% at baseline to –20.2% after HBOT. In the sham group, GLS was –17.8% at baseline and –19.1% at the end of the study, with no statistically significant difference between the two measurements."
No statistically significant difference means we do not know that HBOT works. Since the difference treatment and sham treamtent is negligible.
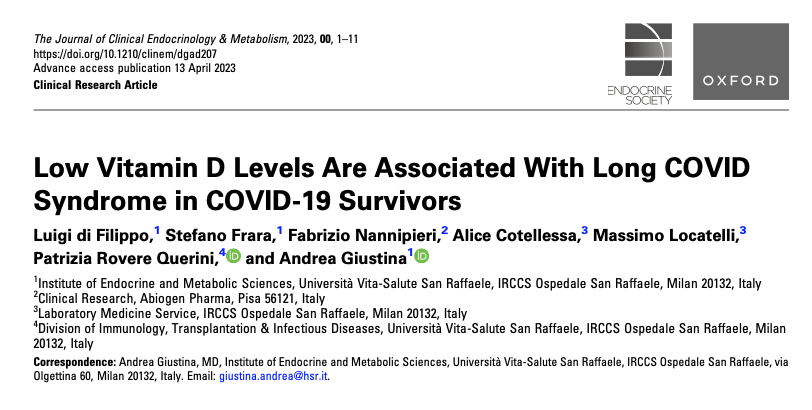
Vitamin D and Long Covid
Long COVID sufferers have lower 25(OH) vitamin D levels than matched patients without long COVID.
It remains to be seen if Vitamin supplementation will imporve LC symptoms. However, for those of us that are not making it outside much, vit D Supplementation is probabaly a good idea.
Sleep Apnea and Long Covid
People with sleep apnea are much more likely to develop Long Covid.
There is a lot of overlap between the symptoms namely fatigue, lack of energy, headache and memory loss.
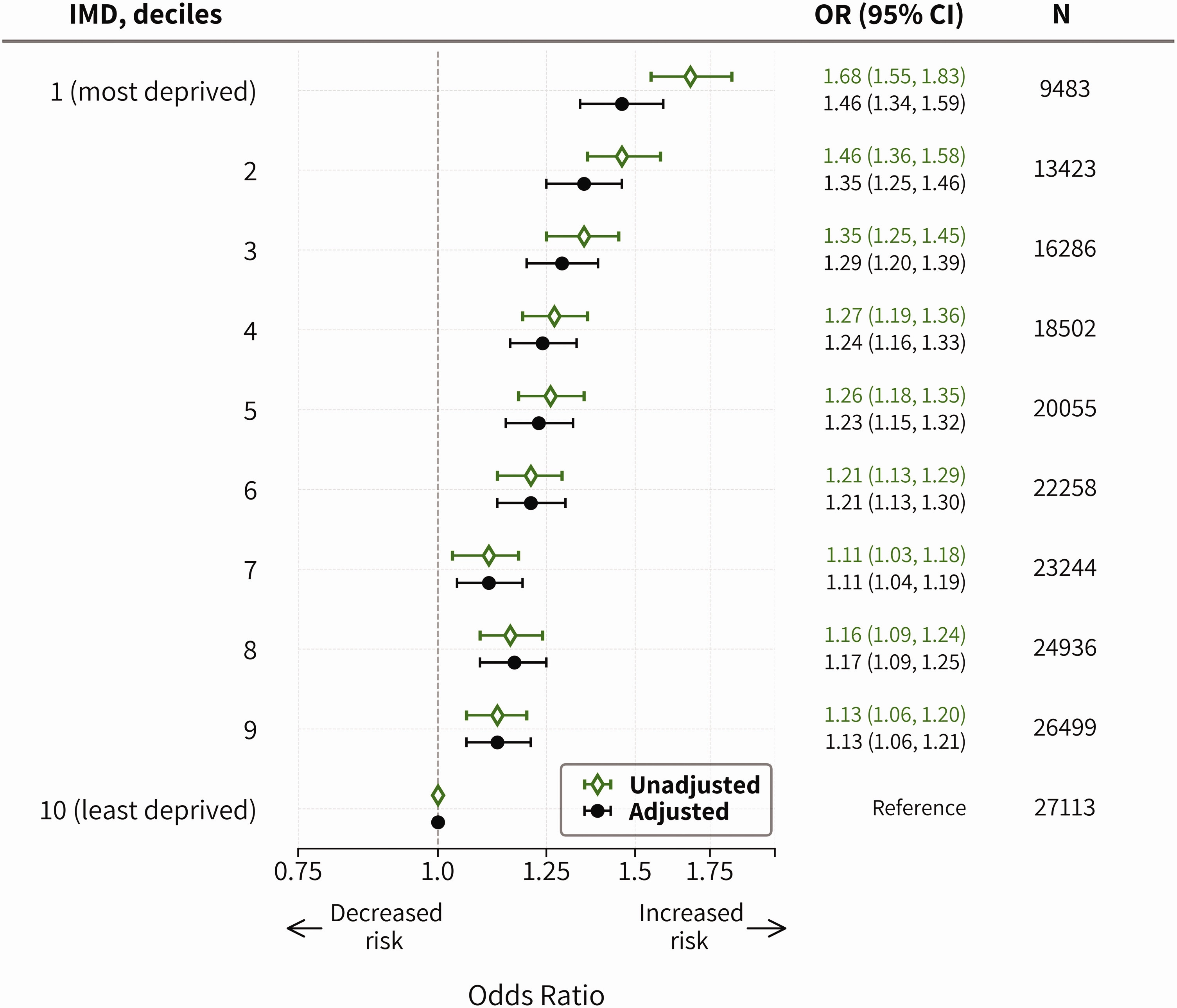
Low Covid more likely if you live in a deprived area.
This UK based estimated the risk of Long COVID by socio- economic deprivation and to further examine the inequality by sex and occupation. To no great surprise it showed LC more likely if you work, in health care, education or social care.
"the odds of Long COVID are 46% higher on average for participants from the most deprived areas compared to those in the least deprived areas."
Clues to causes of long COVID
“The scientists found that levels of a particular set of proteins that are crucial in controlling the growth and activity of immune system cells were almost undetectable among individuals who had long COVID. As a result, the researchers suspect that lungs and other organs are unable to fully heal and fend off other illnesses after being infected with SARS-CoV-2, the virus that causes COVID-19.”
People with long COVID continue to experience medical gaslighting more than 3 years into the pandemic
"In January 2023, our team of researchers at the Pacific Institute on Pathogens, Pandemics and Society published a research brief about how people seek out information about long COVID. The brief was based on a scoping review, a type of study that assesses and summarizes available research...."